The DOE has awarded $5 million to create tools that increase the nation’s preparedness for biological threats — including an infection-rate tracking program for COVID-19 developed by a Sandia team in 2020.
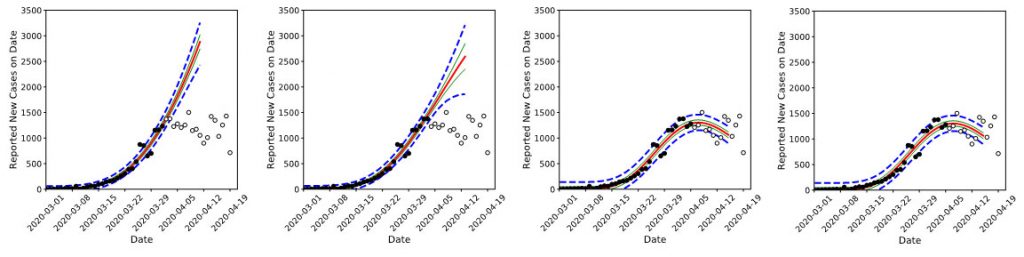
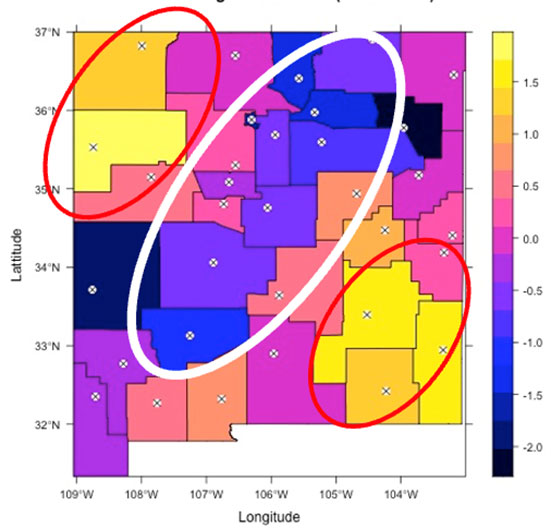
Sandia researchers Jaideep Ray and Cosmin Safta developed an approach using publicly available data from states to track and predict outbreaks of COVID-19 in large populations. Since then, they have refined their model to track infection rates at the county level, where infection rates and case counts start small.
“You may not get hundreds of people infected or coming in sick every day, especially during the early days of an outbreak. You may get 10 to 12, which is what we’ve seen for counties like Bernalillo and Valencia in New Mexico,” Jaideep said. “If you get about five to 10 people coming in sick every day, we can figure out how fast the disease is spreading, and we can forecast how it’s going to move in the next two weeks.”
That kind of specificity is vital to learning to stop outbreaks before they have a chance to spread. In 2020, Jaideep and Cosmin were able to forecast the short-term spread of COVID-19, allowing public health agencies to plan medical resources for epidemiological hotspots.
“Given that humans are now coming into contact with new animal species, which are migrating with the changing climate, there are new diseases that will be coming over to the human species over and over again,” Jaideep said. “This is just the beginning of many potential pandemics. But a pandemic could be detected early and stopped right away before seriously impacting the nation, as COVID-19 did.”
In June, DOE’s Office of Science established a Bio-preparedness Research Virtual Environment initiative to plan for future events and put out a call for proposals to advance work that can provide early warning. The Sandia team partnered with researchers from Argonne National Laboratory. Their joint proposal was accepted in August with a total project award of $825,000 a year.
“The first thing we want to do is try to make the model less computationally expensive,” Jaideep said, explaining the goals for the next two years. “The second thing that we are going to do is look at the question: If you had the beginnings of an outbreak, and it’s infected 30 or so people in a small village of 100 or 200 people, can we use that data to infer the mechanism of human-to-human transmission and what the spread rate is? In other words, does the new disease have the potential to become a pandemic?”
Finally, the team will refine an agent-based modeling tool developed at Argonne. This computational framework looks at individual or group interactions through the lens of game theory, evolutionary programming, sociology and similar analysis methods to model the spread of an outbreak — including scenarios where public health restrictions have been instituted. Such models are invaluable in evaluating the efficiency of potential public health countermeasures in slowing an outbreak versus the disruption they would cause.
“If a disease has traveled across families, can you use data and computer modeling to identify the social links over which it progressed? It’s called tracing the chains of transmission and yields information on the mechanism of transmission — but can you get a computer, rather than public health personnel, to do it?” Jaideep said. “The work at Sandia is very focused on extracting such information from data. Argonne has been at the other end of things, using this information — the rate and mechanism of disease spread — in agent-based modeling to figure out ways in which the disease’s spread could be slowed or stopped, while minimizing the disruption to daily life.”
Jaideep hopes that the combination of the two approaches will allow the labs to model human social interactions on an individual level accurately, perhaps predicting how fast diseases can spread in different situations and what factors might curb the spread of biothreats.
“We’ll be using data to ‘back out’ how fast a novel disease jumps from person to person, and the social links facilitating that transmission. This is something we started 13 or 14 years ago. People are very interested in that kind of work now because it tells you the mechanism and route of disease spread — and therefore a weak link where you could potentially break the chain of transmission.”
Such a breakthrough, funded through this research grant, might one day help the nation avoid the debilitating and deadly impacts of the next pandemic.