New patch detects and stops misplaced radiation
Using a simple concept and a patented Sandia sensor that detects radioactive materials, a team at Sandia has developed a patch to stop damage to healthy tissue during proton radiotherapy, one of the best tools to target certain cancerous tumors.
“This is an important need, especially among pediatric patients,” said Patrick Doty, one of the creators of the patch. Proton radiation therapy is used to send a high dose of radiation into a specific area of the body to disrupt and destroy tumor cells, but the radiation also kills nearby healthy cells. The goal is to be as precise as possible when targeting the radiation, but human movement is an issue especially when dealing with children.
“If you breathe, you move. When your heart beats, you move. You can’t stop those types of motions. And kids are wiggly. You can’t keep them still for long,” Patrick said. “Sometimes doctors must resort to general anesthesia and the treatments sometimes go day after day for six weeks. Imagine going to the hospital and having to be put under every day for weeks. That is not good for anyone, but it’s especially bad for kids.”
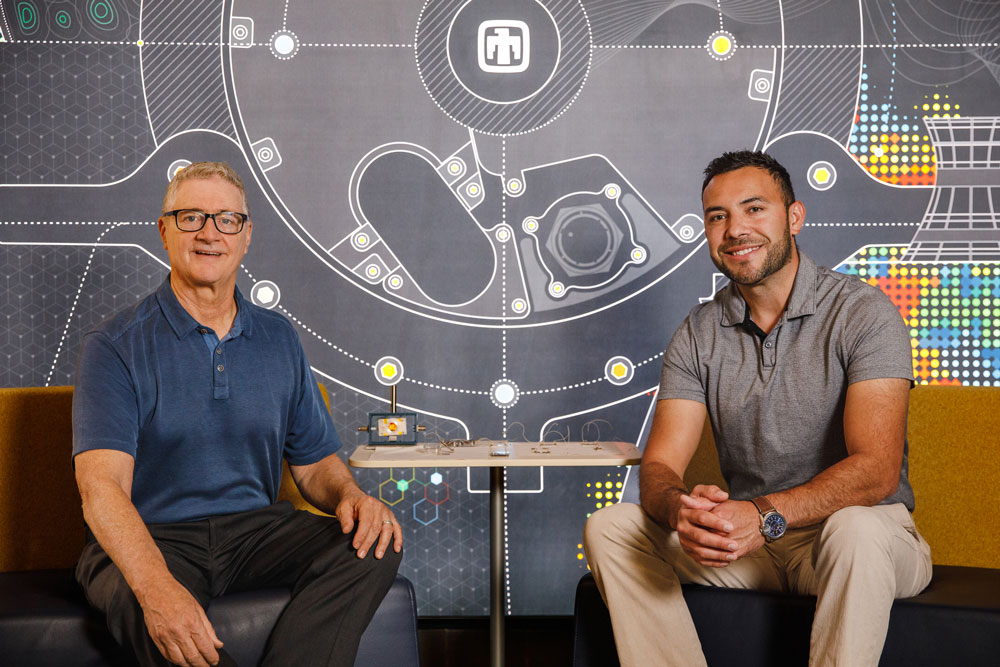
Patrick and fellow materials scientist Isaac Avina came up with a solution: an imaging patch that makes it easier to deliver a precise dose to the right location.
Current systems prompt the radiation to stop when movement is sensed through cameras, but they can’t sense how much radiation was misplaced or at what dosage. Isaac and Patrick said this patch, called an Electronic Polymer Dosimeter for Radiotherapy, can do both.
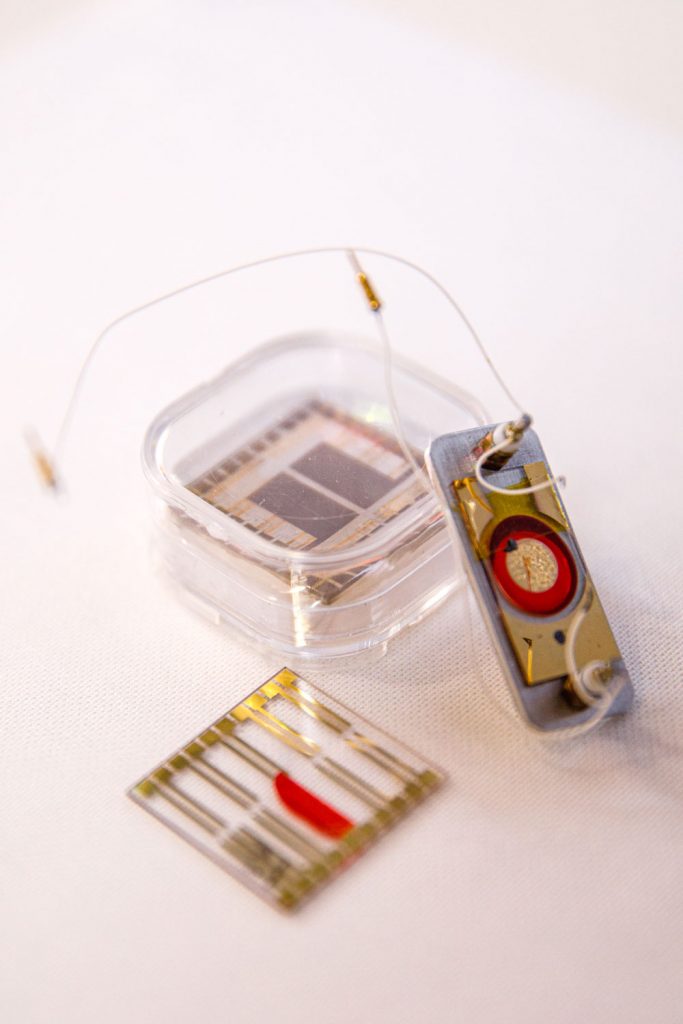
“You can think of this patch as electronic film. The idea is to print an array of sensor elements on the patch and each element or pixel gives location and intensity information. In that way it records an image of the dose delivered,” Patrick said.
Although the team began its focus on pediatric cancer treatment, they quickly learned the patch could be vital in treating other cancers.
“Proton radiotherapy is the gold standard for treating certain cancers, but there are problems with targeting it, especially in small areas like in prostate cancer and brain cancer and now we have a solution,” Isaac said.
“There are certain tissues at risk that you don’t want to destroy, including those in the brain. You can lose hearing because of collateral damage, or you can hit nerves or other vital tissues, so they use physical restraints,” Patrick said. “For brain cancer patients they literally nail a device that fits over your head to a hard bench, so your head is completely still. Imagine how traumatic that is.”
Where the idea came from
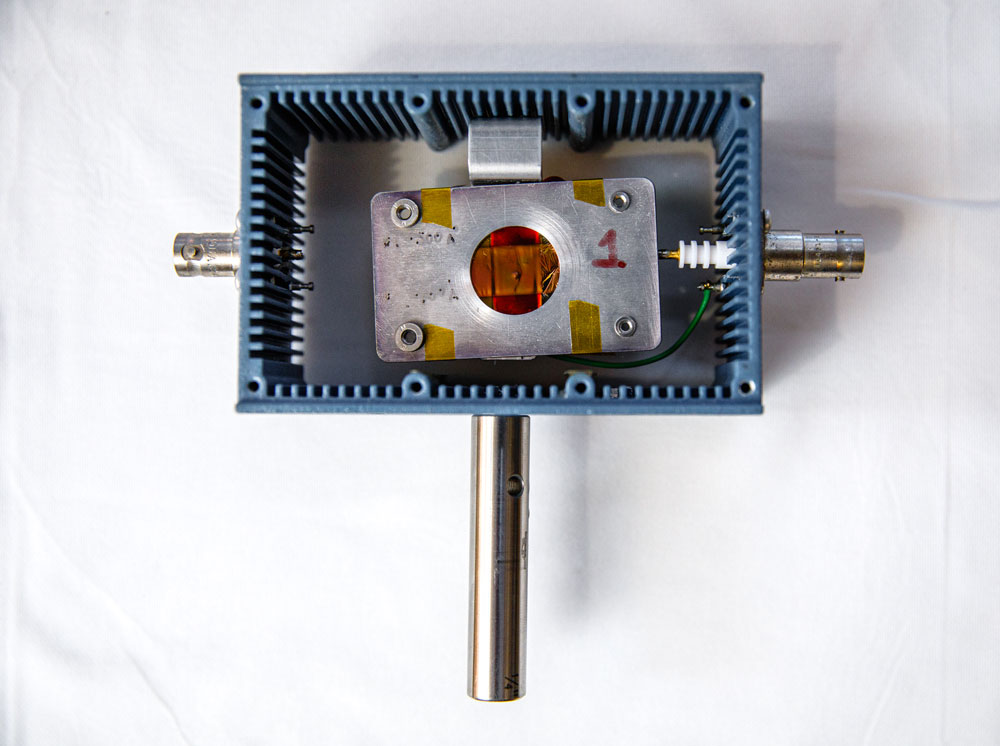
While the team said the need for this new technology is huge, no one has come up with a realistic and inexpensive solution until now. So how did they do it? Isaac and Patrick said the idea stemmed from their nuclear detection work as part of Sandia’s core mission. The main component of this patch is a neutron and proton sensor that Sandia patented.
“It had not been used anywhere else. It was invented here and was designed for detecting signatures from nuclear materials,” Isaac said. “We wanted to see if we could use it for other applications including cancer therapy, knowing cancer therapy has the same signatures.”
Basic principle, basic materials
The team paired the sensor with a polymer and electrodes, attached them to a layered material that looks like a bandage and added adhesive. They say that the polymer, known more commonly as a plastic or resin, is ionized after the proton interacts with it. The electrodes then feed the charge back to an amplifier, detecting the beam intensity and precise location in real time. That stops the radiation if the beam is off target and records the information to determine which tissues the radiation penetrated and at what levels.
Adding artificial intelligence and machine learning tools to the technology may lead to advanced algorithms for treatments. By analyzing the data being gathered by the patch, the sensor can provide more accurate beam profiles that help better differentiate between cancerous and healthy tissue. This can further enhance the efficacy of the treatment and prevent excessive radiation treatments.
A personal mission
For Isaac and Patrick their mission is personal. Isaac’s father is battling cancer, so Isaac learned a lot about cancer treatments and the good and the bad that come with them.
“I wanted to find a way to help this whole process and wanted to contribute but didn’t know how,” Isaac said. “This became especially true while I was researching and talking with the clinics and learned what children have to undergo during these cancer treatments. I realized there was a gaping need in this field of oncology, and I wanted to help.” That’s when Patrick and Isaac teamed up and started brainstorming.
Patrick has been working on radiation detection for more than 20 years and has long been looking for a new way to use the technology. He realized the need in oncology when he and Isaac were accepted into DOE Energy I-Corp, which helps scientists become entrepreneurs. Oncologists from some of the top cancer centers in the country shared the challenges they face in treatment.
“To be able to talk to doctors, who use this every day in the field and find out what their real needs are, we realized just how important this was,” Patrick said.
What’s next
The team has been presenting its technology through various programs and networking with entrepreneurs in hopes of commercializing the patch. They also have seen a lot of interest in testing the technology in situations that are closer to real life. They say some of the country’s top cancer centers have the capability to do so through systems that mock-up an entire proton radiation therapy procedure.
“I was talking to a doctor from one oncology department, and he asked me if I could send it over immediately. He didn’t care about the cost. He didn’t realize that we don’t have any product on hand to share but the urgency was clear. He wanted it not tomorrow but yesterday,” Isaac said.
The team hopes their work can soon change the lives of cancer patients for the better.
“For years we knew that we had a very cool material that did things that nothing else could,” Isaac said. “We wanted to help in another area. We realized that is in cancer therapy.”