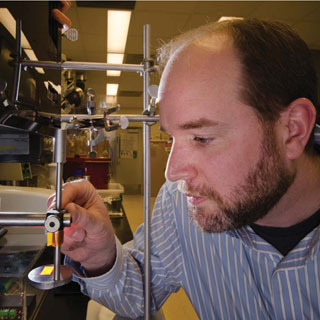
Organic materials chemist Shawn Dirk (1821) focuses a projector during work on neural interfaces, which are aimed at improving amputees’ control over prosthetics with direct help from their own nervous systems. Focusing prior to exposing polymers ensures that researchers pattern the desired feature sizes for the interfaces. (Photo by Randy Montoya)
Sandia researchers, using off-the-shelf equipment in a chemistry lab, have been working on ways to improve amputees’ control over prosthetics with direct help from their own nervous system.
Organic materials chemist Shawn Dirk (1821), robotics engineer Steve Buerger (6533), and fellow researchers are creating biocompatible interface scaffolds. The goal is improved prosthetics with flexible nerve-to-nerve or nerve-to-muscle interfaces through which transected nerves can grow, putting small groups of nerve fibers in close contact to electrode sites connected to separate, implanted electronics.
Neural interfaces operate where the nervous system and an artificial device intersect. Interfaces can monitor nerve signals or provide inputs to let amputees control prosthetic devices by direct neural signals, the same way they would control parts of their own body.
Sandia’s research focuses on biomaterials and peripheral nerves at the interface site. The idea is to match material properties to nerve fibers with flexible, conductive materials that are biocompatible so they can integrate with nerve bundles.
“There are a lot of knobs we can turn to get the material properties to match those of the nerves,” Shawn says.
Researchers are looking at flexible conducting electrode materials using thin evaporated metal or patterned multiwalled carbon nanotubes.
The crux of the problem
Robotics approached the problem from a technical point of view, looking at improving implantable and wearable neural interface electronics. But Steve says that didn’t deal with the central issue of interfacing with nerves.
Working with Shawn’s team “goes after the crux of the problem,” he says.
The challenges are numerous. Interfaces must be structured so nerve fibers can grow through. They must be mechanically compatible so they don’t harm the nervous system or surrounding tissues, and biocompatible to integrate with tissue and promote nerve fiber growth. They also must incorporate conductivity to allow electrode sites to connect with external circuitry, and electrical properties must be tuned to transmit neural signals.
Shawn presented a paper on potential neural interface materials at the recent Boston meeting of the Materials Research Society, describing Sandia’s work in collaboration with the University of New Mexico and MD Anderson Cancer Center in Houston. Co-authors are Steve, UNM assistant professor Elizabeth Hedberg-Dirk, UNM graduate student and Sandia contractor Kirsten Cicotte, and MD Anderson’s Patrick Lin and Gregory Reece.
The researchers began with a technique first patented in 1902 called electrospinning, which produces nonwoven fiber mats by applying a high-voltage field between the tip of a syringe filled with a polymer solution and a collection mat. Tip diameter and solution viscosity control fiber size.
Collaborating with UNM’s Center for Biomedical Engineering and department of chemical engineering, Sandia researchers worked with polymers that are liquid at room temperature. Electrospinning these liquid polymers does not result in fiber formation, and the results are sort of like water pooling on a flat surface. To remedy the lack of fiber formation, they electrospun the material onto a heated plate, initiating a chemical reaction to crosslink the polymer fibers as they were formed, Shawn says. Researchers were able to tune the conductivity of the final composite with the addition of multiwalled carbon nanotubes.
The team electrospun scaffolds with two types of material — PBF, or poly(butylene fumarate), a polymer developed at UNM and Sandia for tissue engineering, and PDMS, or poly(dimethylsiloxane).
PBF is a biocompatible material that’s biodegradable so the porous scaffold would disintegrate, leaving the contacts behind. PDMS is a biocompatible caulk-like material that is not biodegradable, meaning the scaffold would remain. Electrodes on one side of the materials made them conductive.
The work is in the early stages and it would be years before such materials could be used. Studies must confirm they function as needed; then they would face a lengthy Food and Drug Administration approval process.
But the need is there. The Amputee Coalition estimates 2 million people in the United States are living with limb loss. The Congressional Research Service reports more than 1,600 amputations involving US troops between 2001 and 2010, more than 1,400 of them associated with the fighting in Iraq and Afghanistan. Most were major limb amputations.
Before joining Sandia, Steve worked with a research group at MIT developing biomedical robots, including prosthetics. Sandia’s robotics group was developing prosthetics before his arrival as part of DOE-sponsored nonproliferation projects dealing with humanitarian programs.
Patents applied for
Sandia’s work was done under a late-start Laboratory Directed Research & Development (LDRD) project in 2010; afterward, the researchers partnered with MD Anderson for implant tests. Sandia and MD Anderson now are seeking funding to continue the project, Shawn says.
Steve says they are using their proof-of-concept work to obtain third-party funding “so we can bring this technology closer to something that will help our wounded warriors, amputees and victims of peripheral nerve injury.”
Sandia and UNM have applied for a patent on the scaffold technique. The Labs also filed two separate provisional patent applications, one in partnership with MD Anderson and the other with UNM, and expects to submit full applications this year.
The MD Anderson collaboration came about because then-Sandian Dick Fate, an MD Anderson patient who’d lost his left leg to cancer, thought the hospital and the Labs were a natural match. He brokered an invitation from Sandia to the hospital, which led to the eventual partnership.
Dick, who retired in 2010, views the debilitating effect of rising health care costs on the nation’s economy as a defense- and security-related issue.
“To me it seems like such a logical match, the best engineering lab in the country working with the best medical research institution in the country to solve some of these big problems that are nearly driving this country bankrupt,” he says.
After Sandia researchers came up with interface materials, MD Anderson surgeons sutured the scaffolds into legs of rats between a transected peroneal nerve. After three to four weeks, the interfaces were evaluated.
Getting the feature size down
Samples fabricated from PBF turned out to be too thick and not porous enough for good nerve penetration through the scaffold, Shawn says. PDMS was more promising, with histology showing the nerve cells were beginning to penetrate the scaffold. The thickness of the electrospun mats, about 100 microns, were appropriate, Shawn says, but weren’t porous enough and the pore pattern wasn’t controlled.
The team’s search for a different technique to create the porous substrates led to projection microstereolithography, developed at the University of Illinois Urbana Champaign as an inexpensive classroom outreach tool. It couples a computer with a PowerPoint image to a projector whose lens is focused on a mirror that reflects into a beaker containing a solution.
Sandia researchers set up the system with a Dell laptop and an Epson projector. Shawn says they initially tried using a mirror and a 3X magnifying glass, but abandoned that because it produced too much distortion. They now use the magnifying glass to focus UV light onto the PDMS-coated silicon wafer to form thin porous membranes.
While the lithography technique is not new, “we developed new materials that can be used as biocompatible photo-crosslinkable polymers,” Shawn says.
The technique allowed the team to create a regular array of holes and to pattern holes as small as 79 microns. Now researchers are using other equipment to create more controlled features.
“It’s exciting because we’re getting the feature size down close to what is needed,” Steve says.